Radiation therapy, or radiotherapy, is a type of cancer treatment in which specialists kill cancerous cells in the body by exposing them to ionizing radiation, such as X-rays, gamma rays, high-energy electrons or heavy particles. It is one of the most widely used cancer treatments, with around half of all patients requiring radiotherapy at some point during the course of the disease.
What is Radiation Therapy?
Image showing external radiotherapy, or teletherapy, which is one of the common treatments for cancer. (Graphic: A. Vargas/IAEA)
How does radiation therapy work against cancer?
Cancer is a condition in which cells in a specific part of the body begin to grow and reproduce uncontrollably, forming tumours which affect surrounding tissues and organs and sometimes spread to other parts of the body through the bloodstream or lymphatic system.
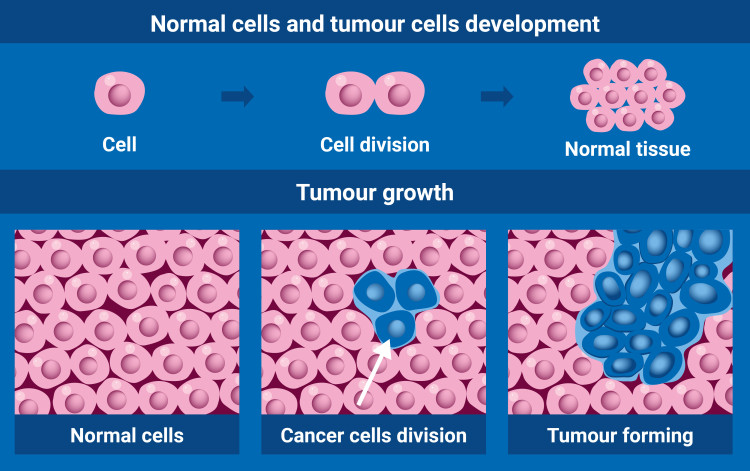
(Graphic: A. Vargas/IAEA)
Radiotherapy involves using carefully selected doses of ionizing radiation to damage the DNA of cancer cells. The DNA controls how they divide. Radiation causes the tumour to shrink and, in some cases, die. Radiation therapy has been used since the 1890s to treat almost all types of cancer. It is applied alone or in combination with other treatments, such as chemotherapy or surgery, to cure cancers or control symptoms of the disease.
Types of radiation therapy
Depending on the type and location of cancer, radiation oncologists use two types of radiation therapy, alone or in combination: external, also known as teletherapy, and internal, or brachytherapy.
The selected treatment needs a team of qualified experts, consisting of a radiation oncologist, medical physicist and radiation therapy technologist, who use radiation to destroy the tumour while minimizing harm to healthy cells.
Teletherapy
The most common type of radiation therapy is teletherapy, whereby radiation is delivered to the tumour area in the form of a high-energy beam. This radiation is emitted from a machine located at a distance from the body, such as a cobalt unit or a linear accelerator.
During the therapy, the patient lies motionless on a table while the machine moves around the body, directing precise doses of radiation at the tumour from several angles. The beam size and shape are carefully adjusted to deliver the dose to the tumour while sparing the normal tissues.
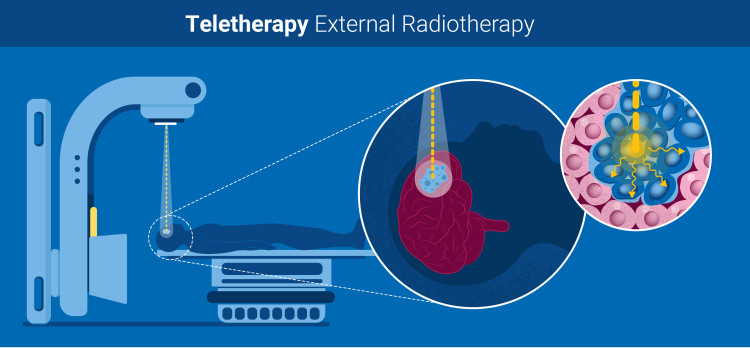
External radiotherapy is used to treat many types of tumours, including in the head, neck, breast, lung or colon. (Graphic: A. Vargas/IAEA)
Brachytherapy
With brachytherapy, a small encapsulated radioactive source is placed inside the body, enabling a high dose of radiation to be delivered directly to the tumour with only minimal impact on the surrounding tissues.
The source can be placed either temporarily or permanently. For temporary application, a capsule containing caesium, iridium or cobalt sources is inserted through a needle or a special applicator. Depending on the dose delivered by the source, the capsule can remain in the body for several minutes to several days. For permanent application, an implant – one example of which is iodine-125 and is usually about the size of a rice grain – is inserted into the body and targets the tumour with radiation, before losing its radioactivity over time.

Brachytherapy is often used to treat prostate, breast, skin and some head and neck cancers. (Graphic: A. Vargas/IAEA)
How effective is radiotherapy?
Radiotherapy is a highly effective and well-established treatment that millions of patients undergo every year for brain, breast, head and neck, cervical, prostate, skin and other cancers. The effects of the therapy can be seen over time, rather than immediately, and it can take days, weeks or months after the end of the treatment to see the impact of the radiotherapy on the tumour.
Some of the latest advances in radiotherapy, including 3-D conformal radiotherapy, intensity-modulated radiotherapy and image-guided radiotherapy, help define the target area with high accuracy and effectively deliver precise doses of radiation, causing only minimal damage to healthy cells, tissues and organs.
What are the side effects of radiation therapy?
Side effects depend on the amount of radiation used in radiotherapy and the part of the body that has been irradiated. Patients may experience short- and long-term side effects or no side effects at all.
Is radiotherapy safe?
Teletherapy, conducted with specially designed equipment by a team of highly qualified healthcare professionals, is safe. While patients may experience side effects, others, including doctors or family members near the patient during treatment, are not at any risk of radiation.
Teletherapy does not make patients radioactive. The hazards associated with brachytherapy are also minimal. When the radioactive source is put inside temporarily, the patient remains in the hospital, under special conditions to prevent the staff and public from being exposed to radiation. Once the source has been removed, there is no residual radiation in place.
A permanent implant is placed in such a way that the radiation is absorbed by the tumour. To make sure that the radiation levels are sufficiently low, doctors carry out a special check before they release the patient from the hospital.
What is the role of medical imaging in radiotherapy?
Medical imaging plays a crucial role in cancer patient management and is requisite for the planning, delivery and evaluation of radiotherapy treatment. The integration of advanced imaging techniques in radiotherapy has revolutionised cancer care and improved patient outcomes. In this context, the role of medical imaging includes:
Evaluation of disease location and spread
Determining whether the cancer is at an early stage or has spread to other parts of the body is done through medical imaging. Image-guided procedures such as biopsies are minimally invasive and are necessary for accurate tissue diagnosis.
Medical imaging modalities, such as computed tomography (CT), ultrasound, magnetic resonance imaging (MRI) and positron emission tomography (PET), are essential for accurate cancer diagnosis and staging. These techniques help identify the location, size and extent of the tumour, as well as its relationship to adjacent structures and the presence of metastases.
Treatment planning
Imaging is used for treatment planning: from medication and radiotherapy to surgery or, in certain cases, palliation. During radiotherapy planning, medical imaging generates three-dimensional images of the tumour, allowing for better radiation therapy targeting of the tumour while minimising damage to healthy tissues.
Image-Guided Radiotherapy (IGRT) incorporates real-time medical imaging into the radiotherapy process to ensure accurate and consistent delivery of radiation doses.
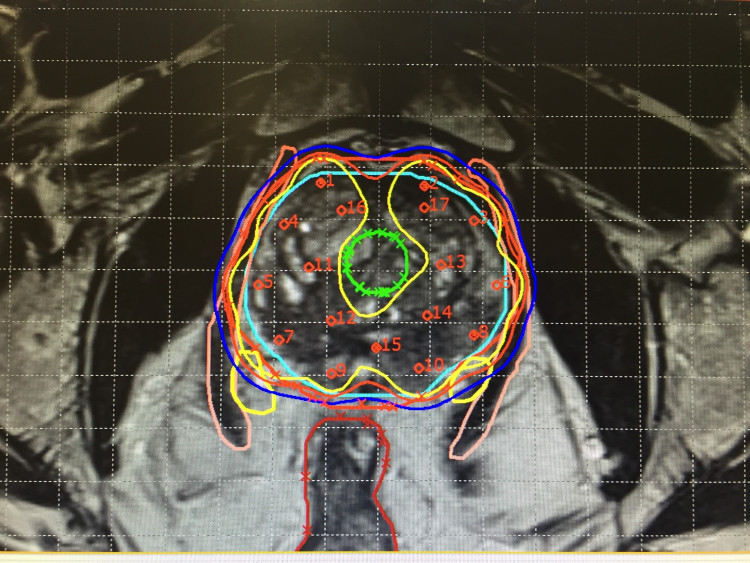
Detailed medical images enable health professionals to distinguish between tumours, healthy tissues and organs to ensure cancer cells are correctly targeted. (Photo: Auna Oncosalud)
What is the role of the IAEA?
- In 2022, the IAEA launched the Rays of Hope initiative to support the establishment and expansion of radiotherapy and medical imaging services for cancer patients. Where most needed, it aims at building capacity for radiation medicine and supporting the provision of training, guidance, technology and quality control to countries that currently have little or no access to radiation therapy. In addition, the Rays of Hope initiative supports the development of Anchor Centres, which are regional centres with the aim of enhancing education, research, training, quality assurance and infrastructure in the region.
- Through its Programme of Action for Cancer Therapy (PACT) and in cooperation with the WHO and other global partners, the IAEA supports countries in enhancing their national cancer care services, facilitating the transfer of scientific knowledge, organizing educational and training activities and providing cutting-edge equipment. The assistance provided by the IAEA has helped many countries to set up and strengthen radiation medicine capabilities, including radiotherapy, radiology and nuclear medicine.
- Since 2004, the IAEA has carried out imPACT Reviews — a unique assessment tool which supports countries in improving comprehensive cancer control. imPACT Reviews assess a country’s cancer care capacities and needs to determine priority interventions necessary for effectively responding to its cancer burden.
- The IAEA helps countries with the safe and effective use of radiation medicine, issuing internationally harmonized guidelines and best practice recommendations on radiation dosimetry. It also assists countries in establishing appropriate occupational radiation norms by providing guidance through its Safety Standards.
- The IAEA has established the Human Health Programme to support Member States in using nuclear techniques to prevent, diagnose and treat cancer. The Programme provides technical expertise in radiation oncology and promotes and coordinates research in clinical radiation oncology and applied radiation biology.
- The IAEA maintains a dosimetry laboratory, which plays a key role in establishing and disseminating best practices in the safe and effective use of radiation for the diagnosis and treatment of cancer. The laboratory offers important quality assurance services related to medical physics and dosimetry, including the calibration of reference standards used for dosimetry measurements and dosimetry auditing services.
- The IAEA hosts the Radiation Protection of Patients (RPOP) platform – the leading resource for health professionals, patients and the public on the safe and effective use of radiation in medicine.
- The IAEA maintains a database, the DIrectory of RAdiotherapy Centres (DIRAC). It is the most comprehensive database on radiotherapy resources, including information on radiotherapy centres, teletherapy machines, brachytherapy units, treatment planning systems, computed tomography systems and simulators.







