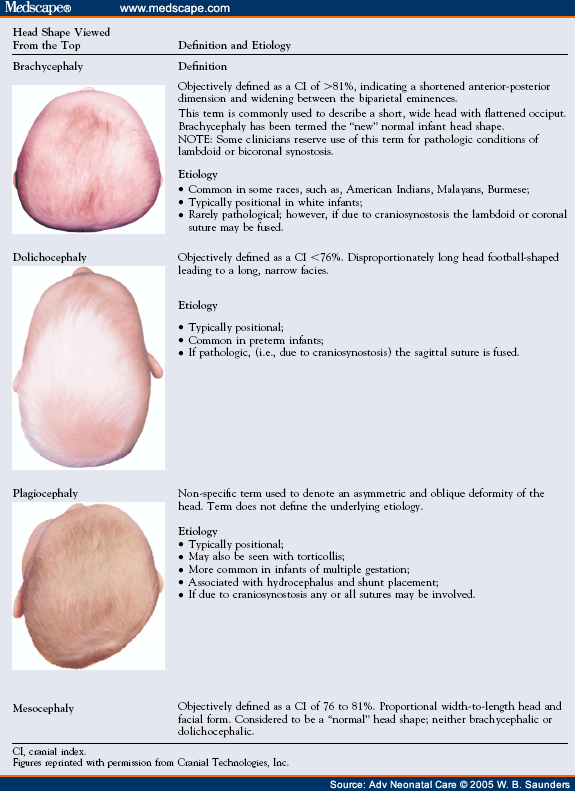
Preventing Positional Plagiocephaly and Dolichocephaly in the NICU
Infant positioning is an important aspect of nursing care and requires ongoing vigilance. In the NICU, positioning options may be limited by the infant's critical medical status and physiologic tolerance of alternative positions. Prone positioning is frequently indicated in sick or premature infants to decrease stress, promote sleep, enhance oxygenation and ventilation, and to improve feeding tolerance.[22,23,24,25] During the acute phase of the illness, medical stability is paramount and head shape concerns are secondary. Whenever possible, nurses should make efforts to choose positions that promote symmetrical cranial shape.
All infants should be transitioned to the supine sleep position before hospital discharge.[26,27,28] Supine sleep positioning models correct "Back-to-Sleep" positioning for parents. An infant that is accustomed to prone sleep may initially have problems sleeping in the supine position. The infant may require an adjustment period, to learn to sleep comfortably supine. This is best accomplished before discharge. Positioning devices, such as blanket rolls, nests, or other means of containment, are not appropriate for use with unmonitored infants, and should be discontinued well before discharge.[29]
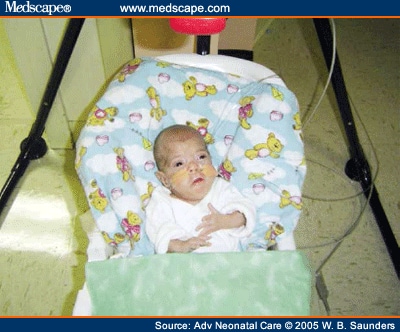
The preterm infant who is placed in the prone position for extended periods may develop pronounced dolichocephaly and a prominent occiput. Limit prone positioning if the infant is dolichocephalic. The dolichocephalic head shape (Fig 4) interferes with the development of midline positioning and head control, causing a persistent preference for the head to fall to either side. In comparison to the full-term infant the preterm infant is also relatively hypotonic, contributing to difficulties in maintaining midline head positioning.
This dolichocephalic preterm infant enjoys time in the upright seated position, promoting midline positioning and head reshaping.
Some critically ill infants may be positioned supine with the head to one side for extended periods. Critical medical status or specific technologies such as extracorporeal membrane oxygenation or high-frequency oscillatory ventilation may prohibit regular repositioning, leading to asymmetric occipital flattening. Deep sedation or chemical paralysis prevents the infant moving and spontaneously repositioning, thus worsening the plagiocephaly. To avoid this, consider alternating positions, rotating the head from one side to the other. In the hospital nurses can support alternative midline positioning by using positioning devices (e.g., gels, wedges, blanket rolls, nesting, or other means of containment) to support the head in the midline position, and redistributing mechanical forces on the occiput (Fig 5).
Midline positioning is maintained in the NICU by utilizing wedges and blanket roles; both are appropriate in a monitored infant.
Positional plagiocephaly occurs more often on the right occiput. The right-sided preference may be in part a result of intrauterine position because 85% of vertex presentations lie in the left occipital anterior position. As the infant's head descends into the pelvis, growth of the right occiput and left frontal areas may be limited, leading to potential development of torticollis and plagiocephaly.[30]
A right-sided preference can be exacerbated by care practices in the NICU and after discharge. Infants need to experience and be supported in a variety of positions. The infant's emerging visual tracking system activates head turning during calm, alert, social interaction time. Because most people are right-handed, nursing care is usually performed from the infant's right side, further encouraging a head preference to the right. Nurses can counteract this by alternately approaching the infant from the left side. Either provide care from the "other side of the bed" or reposition the infant in the bed, head-to-foot, so that the infant must turn his or her head to the left, toward the caregiver.
Breastfeeding naturally promotes alternate head turning as the infant nurses from each breast. Infants who are bottle-fed are most often held in the left arm, promoting persistent head turning to the right. Encourage parents and caregivers to switch the infant to their opposite arm midway through a bottle feeding, or alternate arms with each feeding.
Individualization of care is a core concept of developmental care.[31,32,33] Developmentally supportive positioning should include strategies to prevent plagiocephaly from occurring, and reshape the head if deformations occur. If the head is becoming flattened, a positioning program should be developed to reshape the head. Occupational or physical therapists can evaluate the infant and collaborate with the nurse and parents to develop a treatment plan. Early identification of a preferred head orientation may indicate the presence of neck muscle dysfunction, also called SCM imbalance. A corresponding treatment plan of positioning and stretching may help prevent the progression of positional plagiocephaly.[20,34]
Adv Neonatal Care. 2005;5(6):329-340. © 2005 W.B. Saunders
Cite this: Impacting Infant Head Shapes - Medscape - Dec 01, 2005.








Comments