Immunity in the spotlight: how vaccinations and the immune system protect us
The ongoing SARS-CoV-2 pandemic has put immunology research firmly into the global spotlight, generating tremendous interest in this field. The immune system is the body’s defense against microorganisms and disease-causing cellular changes (such as cancer). We are constantly exposed to a variety of microorganisms present in the environment, such as viruses, bacteria and fungi. Harmful microorganisms are pathogenic, beneficial microorganisms are commensal.
The immune system is complex, with many different parts and components. Scientists at St. Jude are studying these aspects of immunity to gain a better understanding of human health and how we respond to disease.
What comprises the immune system?
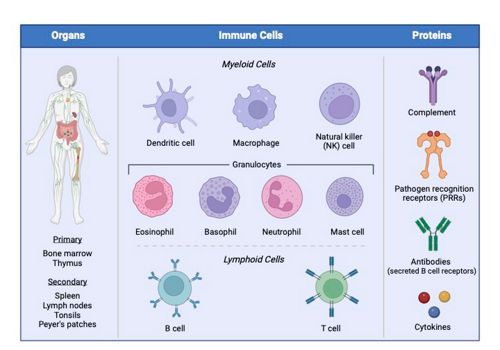
The immune system is comprised of several different organs, types of cells and proteins that have specific functions.
The immune system is composed of organs, cells (commonly called “white blood cells”) and proteins.
- Organs included in the immune system can be divided in two groups: (1) primary lymphoid organs include the bone marrow and thymus, and are sites where immune cells are produced and mature; (2) secondary lymphoid organs include tissues such as the spleen and lymph nodes, and are sites that maintain immune cells and are where adaptive immune responses are initiated.
- Immune cells are collectively referred to as leukocytes. Similar to how our armed forces are comprised of multiple branches, each with distinct functions, but the collective goal of protecting our country; there are many types of leukocytes, each with a unique set of functions, but which work together to defend our body against harm. Myeloid cells are the frontline troops of the immune system, and include macrophages, dendritic cells, natural killer cells and granulocytes. Lymphocytes are the immune system’s elite special operations units, and include T and B cells.
- Immune proteins are the equipment of the immune military. They are involved in every aspect of an immune response and include functions such as pathogen detection, communication between cells, clearance of infected cells and repair of damaged tissue.
How does our immune system protect us from immediate and future harm?
The immune system and its response can be broadly grouped into two categories - innate immunity and adaptive immunity.
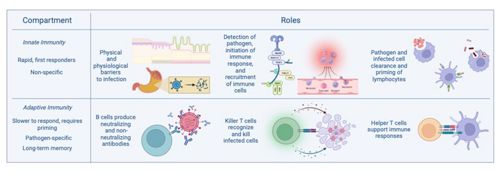
Innate immunity is the first response against disease whereas adaptive immunity is the slower, long-term memory that requires priming.
- Innate immunity is initiated by proteins that detect pathogens, also called pathogen recognition receptors, and myeloid cells that are the “first responders” to a threat. It is a rapid response, and not specific to a particular pathogen. In immediate harm, it functions to detect a pathogen, initiate the appropriate immune response (depending on the class of pathogen) and control the initial pathogen growth to limit host damage.
- Adaptive immunity, the elite special operations units of the immune system, includes lymphocytes, and is the arm of immunity that primarily relays immune memory. In comparison to innate immunity, adaptive immunity is slower to respond because it is pathogen specific and requires priming, or an initial exposure to a pathogen, to initiate. In immediate harm, adaptive immunity clears infected cells and the pathogen itself. Following an initial exposure, memory lymphocytes are established and protect from future harm by responding faster to any subsequent exposures, and, in the case of B cells, produce antibodies, which are proteins that can recognize and effectively neutralize the threat of a pathogen.
What are the goals of vaccination and why do I need one?
The purpose of a vaccine is to initiate the priming step required to establish immune memory, a kind of training exercise for the immune system. Vaccinations are small pieces or weakened, non-harmful versions of a virus, bacteria or infectious agent that are given in small amounts to your body, which alert and train your immune system to protect you against future infections with the same agent.
Vaccines teach our immune systems to memorize harmful agents and respond to them quickly if seen again. In this way, vaccines act like an immunologic wanted poster informing your T and B cells who the bad guys are.
The goal of vaccines may be different based on the disease type, but in general, nearly all vaccines are designed to prevent disease severity. Some vaccines are also formulated to reduce disease transmission or reduce the total number of days sick.
One very important aspect to remember about vaccines is that they are not a physical shield preventing you from being exposed to a bacteria or virus, but rather, work with your immune system to reduce or eliminate harm after exposure. Additionally, if you experience symptoms after receiving a vaccine, this is completely normal and a good sign that your immune system has recognized and is responding to the vaccine.
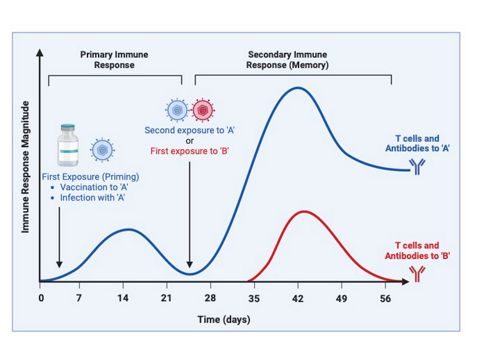
The immune response initiated from initial exposure (blue line days 0-26) is substantially smaller compared to a secondary exposure to the same pathogen (blue line days 27-58). However, when a pathogen evolves to the point that it looks sufficiently different from its original version (virus B versus virus A), it can evade pre-existing immunity and the immune response that is induced is essentially an initial exposure (red line days 34-58).
What have vaccines eliminated or reduced?
Vaccines have helped substantially reduce and/or effectively eradicate numerous illnesses. For example, in the 20th century (1900-2000) the annual morbidity for measles was 530, 217 whereas in 2021 the annual morbidity for measles was 9, that’s a 99% decrease due to vaccination.
In pandemics, vaccines can help manage the health care burden by reducing illness severity. Pandemic causing microorganisms include Ebola virus, influenza virus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and more. Ongoing research also aims to develop vaccines against mutated versions of viruses that haven’t yet occurred.
Why is more than one vaccine sometimes necessary?
Multiple vaccines are generally needed for three reasons:
- Multiple vaccines may be required to meet a threshold of immune response that is required to protect against infection or severe illness.
- Memory immune responses naturally wane over time. Booster vaccines are intended to boost the memory immune response back to the threshold required for protection
- Pathogens naturally change through multiple mechanisms, and this can result in a pathogen that looks different from the initial version, so much so that the immune system no longer recognizes it.
T cells in vaccination
T cells are a type of white blood cell derived from the bone marrow and are members of the adaptive arm of the immune system. T cells help clear active infections, fight cancer and can be trained by a vaccination or infection to protect us against future attacks.
Similar to how a lock recognizes a key, T cells help our bodies fight infections by recognizing small fragments of a pathogen with a complex of proteins that are collectively called a T cell receptor (TCR). This receptor is what gives a T cell its specificity, which leads to its activation and function.
There are also different types of T cells, which protect us in unique ways. T ‘Helper’ cells use their TCRs to train other immune cells, such as aiding B cells to produce antibodies. During an ongoing infection, a second type of T cell, called ‘Killer’ T cells, use their TCRs to recognize infected cells and eliminate them along with any pathogens inside. These Killer T cells also detect and attack cancerous tumor cells.
How are T cells different from antibodies?
T cells elicit their protective effects by acting on other cells (Figure, panel B), which is why their responses are referred to as cell mediated immunity. In contrast, B cells produce antibodies which circulate in the bloodstream, and act on the pathogen itself. Protection conferred by antibodies is referred to as humoral immunity. Antibodies generally function by:
- Binding to a pathogen and preventing it from binding to and infecting host cells (neutralization).
- Helping the immune system “see” the pathogen (opsonization), thereby inducing removal of the pathogen.
- Stimulation of additional immune responses.
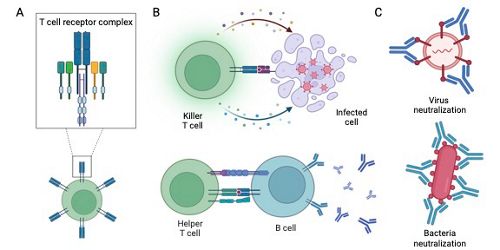
(A) A T cell, zoomed in on the T cell receptor complex. (B) Top: Killer T cells acting on an infected cell and inducting cell death. Bottom: Helper T cell acting on a B cell and assisting with antibody production. (C) Antibody neutralization of pathogens.
Can we target T cells in vaccine design?
Absolutely! Vaccine efficacy varies depending on the pathogen it targets. Part of the challenge in achieving a highly and broadly effective influenza vaccine is its propensity to mutate (as described above). New, or next generation vaccines, seek to improve multiple aspects of vaccine design to achieve optimum vaccine efficacy. For instance, a neat aspect about T cell function, as it pertains to infectious diseases, is that they target proteins that are less prone to mutation, meaning they target the most important pathogen proteins that are unlikely to change and avoid future immune responses. Modifying vaccination strategies to optimize T cell responses is a promising approach to designing broadly effective vaccines that can recognize viruses even when they mutate. Scientists can also apply vaccination concepts from infectious diseases to other illnesses, such as cancer.
T cell studies at St. Jude
Scientists at St. Jude investigate fundamental concepts of T cell biology to develop new therapeutic options and improve existing treatments. Examples of such treatments include custom designing T cells with receptors that recognize and kill cancer cells, also known as chimeric antigen receptor (CAR) T cells. Join us and learn more in upcoming articles that will expand on T cell development and delve into the exciting, groundbreaking research being conducted at St. Jude!
- The laboratories of Drs. Stephen Gottschalk, Giedre Krenciute, Christopher DeRenzo and Paulina Velasquez develop cellular immunotherapies by designing T cells that recognize and kill cancer cells.
- The Paul Thomas lab specializes in T cell recognition, activation and function in health and disease, such as cancer and respiratory virus infection.
- The laboratories of Drs. Yongqiang Feng and Benjamin Youngblood investigate epigenetic regulation of T cell function and response longevity.
- The Hongbo Chi lab explores the relationship between cellular metabolism and the immune response to identify potential therapeutic targets.
All images created with Biorender.