Euglobin Lysis Time
Euglobin Lysis Time
Euglobin Lysis Time
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
TEST<br />
Euglobulin <strong>Lysis</strong> <strong>Time</strong><br />
METHOD<br />
TEST EVALUATION<br />
Don Jacobs, M.D.<br />
Venous blood is collected in a plasticized tube containing sodium citrate<br />
(approximately 1 part citrate/9 parts plasma). Platelet poor plasma is obtained by<br />
centrifugation at 4C. The plasma is diluted with distilled H2O (1:10) and acidified<br />
by the addition of acetic acid or CO2 to a pH of 5.9. This step causes precipitation<br />
of the euglobulins: plasminogen activators, plasminogen, plasmin, fibrinogen,<br />
factor V, and factor VIE. The inhibitors of fibrinolysis (anti-activators and antiplasmins)<br />
remain in the supernatant and are discarded. The euglobulin pellet is<br />
resuspended in buffer solution. Thrombin or calcium is added to the euglobulin<br />
suspension to form a clot. The specimen is incubated in a 37° water bath and<br />
observed every fifteen minutes until clot lysis is complete. Normal values are<br />
between 3 and 20 hrs. <strong>Lysis</strong> times less than 1 hour are indicative of severe<br />
fibrinolysis. The significance of an elevated lysis time has not been fully evaluated.<br />
The spontaneous fibrinolytic activity of plasma may be mathematically expressed as<br />
1000/ECL time (min).<br />
The significance of an elevated lysis time has not been fully evaluated.<br />
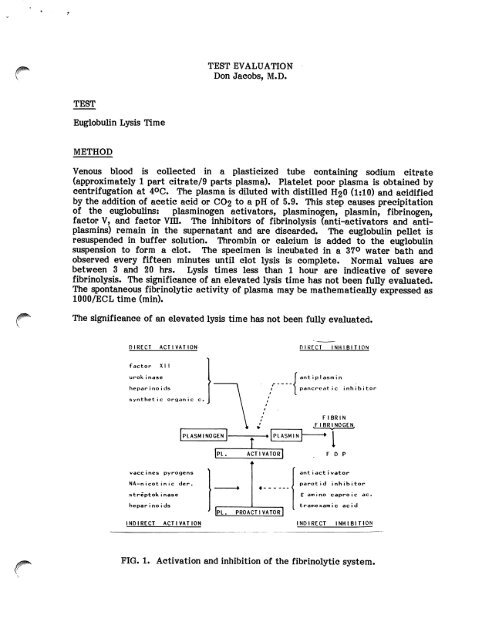
DIRECT ACTIVATION<br />
f a c t o r X I I<br />
urokinase<br />
hepar i no i ds<br />
s y n t h e t i c o r g a n i c c .<br />
v a c c i n e s p y r o g e n s<br />
N A - n i c o t i n i c d e r .<br />
s t r e p t o k i n a s e<br />
hepar i no i ds<br />
INDIRECT ACTIVATION<br />
PLASMINOGEN<br />
PL.<br />
» r<br />
ACTIVATOR<br />
*<br />
PLASMIN<br />
4 <<br />
Ipl. proactivatorI '<br />
DIRECT INHIBITION<br />
ant i pI asm i n<br />
p a n c r e a t i c i n h i b i t o r<br />
FIBRIN<br />
.FIBRINOGEN,<br />
-I<br />
F D P<br />
ant i act i vator<br />
parotid inhibitor<br />
£ a m i n o c a p r o i c a c .<br />
t r a m e x a m i c a c i d<br />
INDIRECT INHIBITION<br />
FIG. 1. Activation and inhibition of the fibrinolytic system.
INTRODUCTION<br />
Page 2<br />
The fibrinolytic system is a critical regulator of fibrin deposition and thrombosis.<br />
The components of the system are diagrammed above. Plasminogen, probably<br />
synthesized in the liver, is a circulating inactive proenzyme which is found in<br />
concentrations of 10-15 mg/dl. Plasminogen is converted into the active serine<br />
protease plasmin by a variety of plasminogen activators. These activators are<br />
widely distributed in a variety of tissues (tissue activator), plasma (activated<br />
Hageman factor/Kallikrein system) and urine (Urokinase). In addition to endogenous<br />
activators, a variety of bacterial products and pyrogens interact with the<br />
fibrinolytic system. The plasminogen activator of greatest physiologic importance<br />
is the tissue activator synthesized in venous endothelium and the vasa vasorum of<br />
muscular arteries. The release mechanism of the vascular-derived activator is<br />
poorly understood. To counterbalance the powerful proteolytic effects of plasmin,<br />
there are numerous fibrinolytic inhibitors which are normally present in<br />
approximately 30-fold excess concentration. These circulating anti-plasmins and<br />
anti-activators include alpha-1-antitrypsin, alpha-2-macroglobulin, antithrombin m,<br />
Cl-inhibitor, and alpha-2-anti-plasmin.<br />
The spontaneous fibrinolytic activity of blood may be measured by simply observing<br />
the time for clot lysis of whole blood collected in a glass tube (Whole Blood Clot<br />
<strong>Lysis</strong> <strong>Time</strong>). Due to the presence of natural inhibitors of fibrinolysis, clot lysis will<br />
occur only in cases of profoundly elevated fibrinolysis. In the Dilute Plasma Clot<br />
<strong>Lysis</strong> Test, dilution of the plasma results in differential depression of the inhibitors<br />
/#^ and allows lysis to occur in normal subjects or cases of slightly elevated fibrinolysis.<br />
^ The lysis time will generally be 18-24 hours. The ECL test is based on the<br />
concentration and precipitation of the fibrinolytic factors in the "euglobulin'1<br />
fraction with removal of the fibrinolytic inhibitors in the supernatant. Thus with<br />
most inhibitors removed, lysis time will be shortened. The ECL test is felt to<br />
reflect the spontaneous fibrinolytic activity of plasma and most closely corresponds<br />
to the level of plasminogen activators.<br />
TECHNICAL PROBLEMS<br />
Fibrinolytic activity is increased when plasma comes in contact with glass, probably<br />
due to the activation of the Hageman factor /Kallikrein system which is capable of<br />
generating plasmin. Thus, glass contact must be minimized. Venous occlusion is<br />
known to cause release of plasminogen activators from venous endothelium and<br />
particular attention to blood drawing technique is necessary. The method of<br />
precipitation of the euglobulin fraction is critical and the ECL times will change<br />
significantly with slight variations in pH and plasma dilution. Most (62%) of the<br />
fibrinogen is precipitated with the euglobulins, but this will vary if pH is not<br />
controlled. Some anti-plasmin activity, probably Cl-inactivator, will co-precipitate<br />
with the euglobulins even if pH and ionic strength of the plasma dilution are<br />
carefully standardized. A recent modification of the ECL test utilizes the addition<br />
of sodium flufenamate to the euglobulin fraction to neutralize any remaining Clinactivator<br />
(not done in the UCSF lab). Precipitation of euglobulins in the presence<br />
of dextran sulfate polymer will markedly increase the recovery of plasminogen<br />
activator and pro-plasminogen activator. Heparin and EACA (epsilon-amino-caproic<br />
acid) remain in the supernatant. Most authors strongly advise against storage of the
Page 3<br />
plasma prior to test performance. Storage at 20°C or 36°C will markedly decrease<br />
fibrinolytic activity. However, storage at -20°C may not affect outcome. For<br />
reproducible results, the test should probably be run within two hours of blood<br />
collection. The type of anticoagulant used will affect results. Citrate is<br />
recommended. EDTA will increase fibrinolysis whereas heparin will reduce it.<br />
Variations in the ECL time will occur with alterations in the fibrinogen level since<br />
the patient's fibrin clot is the substrate in the assay. Care should be taken to avoid<br />
undue handling of the tubes during performance of the ECL test. The endpoint<br />
(complete clot dissolution) is usually easy to read, although difficulties may occur in<br />
lipemic sera.<br />
CLINICAL APPLICATIONS<br />
The ECL test and related assays have been used to investigate a variety of factors<br />
which influence spontaneous fibrinolysis. Epinephrine, stress, and exercise will<br />
markedly increase fibrinolytic activity either by neuronally mediated release of<br />
plasminogen activator or through their effects on vascular permeability. ACTH and<br />
corticosteroids potentiate the effects of epinephrine in stimulating activator<br />
release. Numerous drugs, including procainamide, nicotinic acid, sulfonylureas,<br />
phenformin, reserpine, pitressin, androsterone and DDAVP will increase fibrinolytic<br />
activity. Some of these may find therapeutic application as antithrombotic agents.<br />
Various surgical procedures produce a biphasic response in fibrinolysis. Many<br />
neurologic procedures, including ventriculography and pneumoencephalography, have<br />
been shown to markedly increase spontaneous fibrinolysis and on occasion provoke<br />
severe bleeding. Post-operatively, fibrinolysis usually decreases, reaching a nadir on<br />
postoperative days 1 and 2. Studies have indicated that large rapid falls in<br />
fibrinolytic activity as measured by the ECL test are associated with increased<br />
incidence of post-operative deep venous thrombosis. In approximately 95% of<br />
normal subjects, venous occlusion stimulates fibrinolysis in blood collected from the<br />
occluded vein. This potentiation of fibrinolysis with occlusion is more marked in<br />
arm than in leg veins. Subjects with idiopathic deep venous thrombosis frequently<br />
show no such enhancement of fibrinolysis upon venous occlusion. Release of<br />
plasminogen activators from venous endothelium of occluded vessels may be<br />
physiologically important in controlling thrombosis in situations of stasis.<br />
Fibrinolysis has also been reported to be reduced in individuals with multiple risk<br />
factors for myocardial infarction and in patients with peripheral atherosclerotic<br />
disease, vasculitis, and Raynaud's phenomenon.<br />
Thrombolytic agents such as Urokinase and Streptokinase markedly accelerate<br />
fibrinolysis through direct and indirect mechanisms (see chart). The ECL test was<br />
formerly used to monitor patients receiving thrombolytic therapy for acute<br />
myocardial infarction. Currently, however, only PT, PTT, TT, platelets and<br />
fibrinogen are commonly monitored during intracoronary streptokinase infusion.<br />
The ECL test has been used to monitor patients receiving urokinase therapy for the<br />
treatment of DVT.<br />
The ECL test has been used in the investigation of primary fibrinogenolysis<br />
(hyperplasminemia). Various tissues, including prostate, uterus, and colon appear to<br />
be exceptionally rich in plasminogen activator substances. Surgical manipulation of<br />
these organs may give rise to a consumptive coagulopathy based on widespread
Page 4<br />
intravascular activation of fibrinolysis. Plasmin has a wide range of substrates,<br />
including factors V and VIII, and will interfere with coagulation by multiple<br />
mechanisms. Production of abnormal quantities of plasminogen activator has also<br />
been described in certain tumors and acute leukemias. In primary fibrinogenolysis,<br />
there will be a marked increase in the spontaneous fibrinolytic activity of plasma.<br />
Increased fibrinolytic activity may also be seen, although usually to a lesser extent,<br />
in DIC.<br />
There are no studies providing detailed comparisons of coagulation and fibrinolytic<br />
parameters in primary fibrinogenolysis versus DIC. The utility of the ECL test in<br />
making this distinction is uncertain. In clinical practice, DIC should be ruled out on<br />
clinical and laboratory grounds before primary defects in fibrinogenolysis are<br />
suspected. There is little agreement on the specific clinical indications for<br />
employing the ECL test in general patient management. At present, the test<br />
appears useful mainly as an investigative and research tool. Additionally, the<br />
variety of factors sited above which affect fibrinolysis detract from the specificity<br />
and diagnostic utility of the ECL test.<br />
FURTHER DEVELOPMENTS<br />
In the ECL test, the patient's own fibrin clot serves as the substrate for fibrinolysis.<br />
Different substrates may also be used, including casein (caseinolysis) and synthesis<br />
esters (esterolysis). The most important modification of the ECL time is the Fibrin<br />
^ Plate assay in which a sample of plasma or euglobulin fraction is placed directly on<br />
the surface of a petrie dish containing human or bovine fibrin. At approximately 20<br />
hours, the zone size of fibrinolysis is measured. There is a relatively good<br />
correlation between assays of fibrinolysis as measured in the fibrin plate and the<br />
ECL test. The fibrin plate assay has a more precise and easily quantifiable endpoint<br />
and demands less technician intervention. However, it is not suitable for stat<br />
determinations. A recent modification of the ECL test used the addition of radiolabelled<br />
fibrinogen to the euglobulin fraction. The rate of radioactivity release is<br />
proportional to the fibrinolytic activity of the test plasma. This technique is very<br />
precise and has been used to investigate fibrinolytic activity in families with mild<br />
bleeding tendencies. For many research and clinical purposes, the ECL test has<br />
been supplanted by recently developed assays based on a chromogenic substrate (S-<br />
2251) which is a specific substrate for plasmin and plasminogen activated<br />
streptokinase. Using the chromogenic substrate technique, plasminogen activator,<br />
plasminogen, plasmin, and anti-plasmins may be easily and readily quantified.<br />
REFERENCES<br />
1. Allen RA. Blood sampling techniques for fibrinolytic studies. Thromb Res<br />
23:1-2.<br />
2. Von Kaulla KN, von Kaulla E. "Remarks on the Euglobulin <strong>Lysis</strong> <strong>Time</strong>." In:<br />
JF Davidson (ed.), Progress in Chemical Fibrinolysis and Thrombolysis, Vol 1.<br />
Raven Press: New York, 1975.
fifik^<br />
Page 5<br />
3. Griffiths NJ, et al. Plasma fibrinolytic inhibitors post operation. Surg<br />
Gynecol Obst 144:673-676, 1977.<br />
4. Knight MTN, et al. Fibrinolytic response to surgery. Lancet 2:370-373, 1977.<br />
5. Gader AMA. The potentiating effect of corticosteroids on the fibrinolytic<br />
system in response to I.V. infusion of adrenalin in man. Haemostasis 17:353-<br />
356, 1982.<br />
6. Heimburger N. "Plasminogen Assay: a review and evaluation of various<br />
methods." In: JF Davidson (ed.), Progress in Chemical Fibrinolysis and<br />
Thrombolysis, Vol 1. Raven Press: New York, 1975.<br />
7. Prentice CRM. Basis of antifibrinolytic therapy. J Clin Pathol (Suppl.) 33<br />
(suppl 14) pp. 35-40.<br />
8. Horvath AE. The 125I-Fibrinogen Euglobulin Clot <strong>Lysis</strong> Test. Am J Clin<br />
Pathol 70(2):271-274, 1978.<br />
9. Latallo ZS, et al. Assessment of plasma fibrinolytic system with use of<br />
chromogenic substrate. Haemostasis 7:138-145, 1978.<br />
10. Blix S. Studies on the fibrinolytic system in the euglobulin fraction of human<br />
plasma. Scand J Clin Lab Invest 13(suppl 58), 1961.<br />
11. Arneson H, et al. "A comparison between the ECL time and the fibrin plate<br />
method for the estimation of fibrinolytic activity after venous stasis." In: JF<br />
Davidson (ed.), Progress in Fibrinolysis, Vol 5. Churchill Livingstone:<br />
Edinburgh, 1981.<br />
12. Nilsson IM, et al. "Physiology of Fibrinolysis." In: DL Kline, KNN Reddy<br />
(eds.), Fibrinolysis, CRC Press: Boca Raton, Florida, 1980.<br />
13. Theiss W, et al. Systemic fibrinolytic activity and inhibitor levels during<br />
treatment of deep venous thrombosis with urokinase and streptokinase.<br />
Thrombosis and Haemostasis 5(3):664-668, 1983.<br />
14. Kluft C. Studies on the fibrinolytic system in human plasma: quantitative<br />
determination of plasminogen activator and pro-activator. Thrombosis and<br />
Haemostasis 41:365-383, 1979.<br />
15. Von Kaulla KN, Schultz RL. Methods for evaluation of human fibrinolysis.<br />
Am J Clin Pathol 29:104-112, 1958.